IBS
IBS stands for Irritable Bowel Syndrome, a common gastrointestinal disorder that affects the large intestine (colon). It is a chronic condition characterized by a group of symptoms rather than a specific disease. People with IBS often experience recurring abdominal pain, discomfort, changes in bowel habits, and other digestive issues.
Here are some key points to understand about IBS:
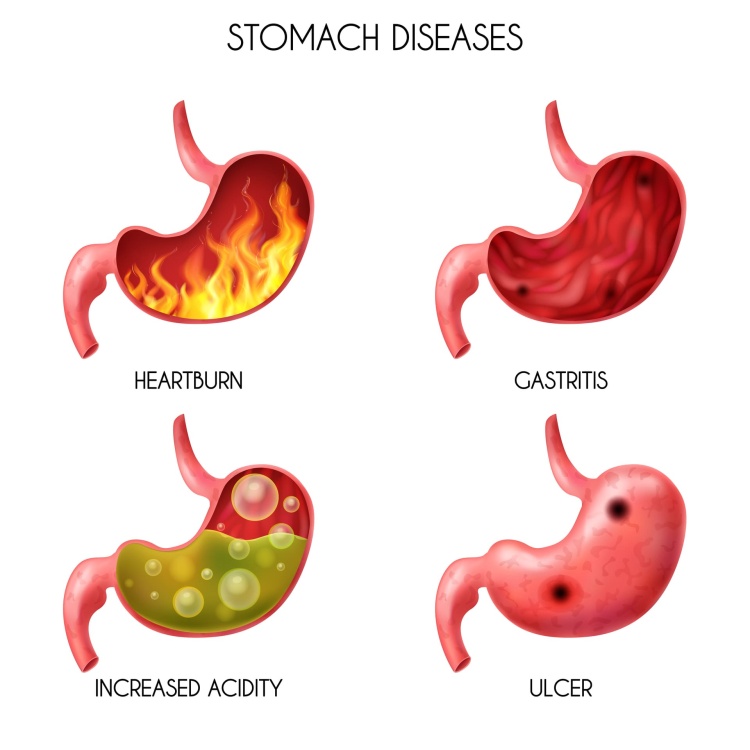
Symptoms: The symptoms of IBS can vary among individuals but commonly include abdominal pain or cramping, bloating, gas, diarrhoea, constipation, or a combination of both. The severity and frequency of symptoms can also vary, with some people experiencing mild discomfort while others may have more severe symptoms that significantly impact their daily life.
Diagnosis: There is no specific test to diagnose IBS, and healthcare providers usually make a diagnosis based on the presence of typical symptoms and by ruling out other underlying medical conditions. They may consider medical history, and physical examination, and may order certain tests to exclude other conditions that mimic IBS symptoms.
Causes: The exact cause of IBS is not fully understood, but it is believed to result from a combination of various factors. These factors may include abnormal gastrointestinal motility (the movement of the intestines), heightened sensitivity to pain in the digestive system, changes in the gut microbiome, and increased reactivity to certain foods or stressors. Psychological factors such as stress and anxiety may also play a role in triggering or exacerbating symptoms.
Triggers: Certain factors can trigger or worsen IBS symptoms in individuals. These triggers can vary from person to person but commonly include certain foods (e.g., fatty or spicy foods, caffeine, alcohol), stress, hormonal changes, medications, and gastrointestinal infections.
Treatment: Although there is no cure for IBS, various approaches can help manage and reduce symptoms. Treatment plans are typically individualized based on the person’s specific symptoms and needs. Some common strategies include dietary modifications (such as identifying and avoiding trigger foods), stress management techniques, medications to alleviate specific symptoms (e.g., antispasmodics, laxatives, anti-diarrheal drugs), and lifestyle changes (e.g., regular exercise, improving sleep habits).
Lifestyle and dietary changes: Making certain lifestyle modifications can often provide relief for individuals with IBS. This may include adopting a balanced and fibre-rich diet, drinking adequate water, regular physical activity, managing stress through relaxation techniques or counselling, and getting sufficient sleep.
Support and self-care: Living with IBS can be challenging, and individuals may benefit from seeking support from healthcare professionals, support groups, or online communities. Keeping a symptom diary to identify triggers and patterns, practising stress management techniques, and finding ways to maintain a healthy overall lifestyle can also be helpful.
It’s important to consult with a healthcare professional if you suspect you have IBS or are experiencing gastrointestinal symptoms. They can provide an accurate diagnosis, offer guidance on management strategies, and help develop an appropriate treatment plan tailored to your specific needs.